What is Obesity?
The American Society for Metabolic and bariatric Surgery defines obesity as a disease in which fat has accumulated to the extent that health is impaired. It is commonly measured by body mass index (BMI), which calculates the relationship of weight to height. Obesity becomes severe obesity when an adult is 100 pounds or more over ideal body weight, has a BMI of 40 or more or has a BMI of 35 or more in a combination with a health-related condition such as obstructive sleep apnea or a disease such as type 2 diabetes or heart disease. Living with excess weight has been shown to put your health at risk. The risk increases sharply as your obesity becomes more severe. Serious health problems may also result when dieting leads to "weight cycling" (the repeated loss and regain of body weight). Bariatric and metabolic surgery has helped thousands of people discover life at a healthier weight and resolve many of the health risks associated with seer obesity.
What is a Body's Set Point?
Body weight and fat levels are regulated by a complex system of signals in your body. These signals control your appetite, digestion, energy balance, and metabolism to keep your body weight and fat at a steady level, or "set point." Your body's set point is part of a basic biological instinct. When your body weight and fat levels fall below your set point, your body activates defense mechanisms to maintain body weight and fat in order to prevent starvation. Everyone’s set point is different and can be changed but because your body works to defend that set point, dieting and exercising are rarely effective in help people with obesity achieve and maintain a healthy weight long-term. When you go on a diet, your body thinks it's being starved and its survival instincts kick in. As a result, your body stores energy-rich body fat, and you can’t lose weight easily. By altering the complex relationship your body has with food and its metabolism, bariatric surgery helps rest your body's ability to effectively manage weight. By altering the anatomy of the stomach and or intestine, these surgeries affect hormonal signals, resulting in decreased appetite, increase feelings of fullness, increase metabolism, and healthier food preferences. These positive changes allow your body to lose weight without the internal fight to return to the higher set point.
Surgical Procedures
Sleeve Gastrectomy
During the sleeve gastrectomy procedure, a thin vertical sleeve of stomach is created using a stapling device. The sleeve is about the size of a banana and typically can hold 50 mL to 150 mL of food. The rest of the stomach is removed. By creating a smaller pouch, a sleeve gastrectomy limits the amount of food that can be eaten at one time, so you feel fuller sooner and stay full longer. As you eat less food, your body will stop storing excess calories and start using its fast supply for energy. Food passes through the digestive tract in the usual order, allowing vitamins and nutrients to be fully absorbed into the body with no postoperative adjustments required to restrict the amount of food passing through the stomach. Like other metabolic surgeries, it also helps to establish lower, heathier body fat set point by changing the signals between the stomach, brain, and liver.

Gastric Banding
The Adjustable Gastric Band wraps around the upper part of the stomach, dividing the stomach into a small upper pouch that holds about one-half cup of food and a larger lower stomach. The degree of band tightness affects how much food you can eat and the length of time it takes for food to leave the stomach pouch. By creating a smaller stomach pouch, the Band limits about of food that can be eaten at one time, so you feel full sooner and stay full longer. As you eat less food, your body will stop storing excess calories and start using its fat supply for energy. The level of the food passage restriction can be adjusted by adding to or removing saline solution from the band through a port that is subcutaneously placed. No part of the stomach or digestive system is stapled, cut or removed; food passes through the digestive tract in the usual order, allowing it to be fully absorbed into the body.

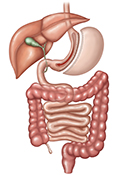
Gastric Bypass
In this procedure, the surgeon creates a small stomach pouch using a stapling device and attaches a section of the small intestine directly to the pouch. This allows food to bypass a portion of the small intestine. By creating a smaller stomach pouch, a gastric bypass limits the amount of food that can be eaten at one time, so you feel full sooner and stay full longer. By bypassing a portion of the small intestine, your body also absorbs fewer calories. As you eat less food and absorb fewer calories, your body will stop storing excess calories and start using its fat supply for energy. Average excess weight loss is generally higher than with gastric banding or sleeve gastrectomy.
Preparing for Bariatric Surgery
Whichever procedure you choose to have, it is important that you begin your new lifestyle preoperatively. Weight loss surgery should be consider one of the tools available to help you lose weight. Making appropriate lifestyle adjustments is crucial to the success of your procedure. Work with your medical team to understand what changes you will need to make in your daily routine to help ensure the success of your surgery. You should understand and agree with your postoperative dietary requirements, exercise needs, and any other changes you will be making before you receive surgery. It is a good idea to implement these changes as well as any other behavior modifications preoperatively to help you transition more easily into your new postoperative lifestyle.
Insurance Guidelines:
Here are several of the most common bariatric surgery insurance coverage requirements:
- Body mass index (BMI) greater than 40 or BMI greater than 35 with comorbidities (eg, diabetes, high blood pressure)
- 18 years of age or older
- Participated in a physician-supervised weight loss program for 3 to 12 consecutive months (depending on insurance plan)
- Documentation of failed diet and exercise plans
- 2 to 5 year weight history with a BMI of 35 or greater with comorbidities
- Separate evaluation from a medical doctor suggesting bariatric surgery
For more information on Bariatric Surgery call (281) 672-5854.